Contraception

We will guide you to choose the contraception method that is best for you.
There are many different contraception methods for women. What method should you use? This varies from person to person.
Side effects of contraception
One cannot tell in advance whether a woman will experience side effects from the contraceptive.
Two women can react completely different to any birth control. The side effects will usually decrease during the first 3 to 6 months.
If you have unpleasant side effects after 3 months, try another brand.
You must consider the positive effects of the contraceptive against the negative side effects.
Some choose to live with mild side effects because they can then enjoy sex without worrying about getting pregnant.
Source: www.sexogsamfunn.no
These are the different types of contraception we offer at our clinic:
Hormonal IUD
The hormonal IUD is made of plastic. It is inserted into the uterus by a midwife. There are three types; Kyleena, which last for five years, Mirena, that lasts for 8 years as well as Jaydess that lasts for three years. If you wish, we can give you local anaesthesia before this procedure.

Depo provera
Depo-Provera contains only the hormone progestin. It prevents pregnancy in the same way as birth control pills.
A syringe is injected into a large muscle, usually in the buttocks, every three months. If more than three months pass between two injections, you are not protected against pregnancy. You’ll have to use a condom until one week after the new syringe has been injected.
FAQ about contraception
Which methods of contraception are available as per today?
There are several different methods of contraception. These differ in terms of effectiveness, user-friendliness, protection against disease, and side effects:
- UD. There are three types on the market: copper IUD, hormonal IUD, two types; Jaydess and Mirena
- Contraceptive Implant
- Birth control pills: combination birth control pills and pure progestogen contraceptives
- Contraceptive patch (Evra)
- Injection (Depo-Provera)
- Vaginal ring (Nuva Ring)
- Condom
- Sterilization: both for men and women
- "Natural Methods": withdrawal method and safe periods
What were the first contraceptives?
The first contraceptive methods came with the arrival of modern rubber technology in the 1900s: condoms and diaphragms. The first IUDs were made of silver and silk in the 1920s, and in the late 1950s the IUD was rediscovered and was made of plastic. Since then, the copper IUD came into medical use in the 1970s and the hormonal IUD in the 1990s. Birth control pills were registered in Norway in 1963.
Which is the most common type of contraception?
Birth control pills are the most common hormonal contraceptive in Norway. Provided it is used correctly, it is highly effective. One disadvantage is that the pill increases the risk of serious side effects, and cannot, therefore, be recommended for all women.
I need highly effective birth control, what's the best option?
There is no method best for everyone; the most important thing is that it is right for you. In terms of effectiveness, the different methods of contraception have varying degrees. IUDs and implants provide the highest effectiveness since they have little or no scope of user error and you don’t have to remember to take it.
Can it be difficult/take long to get pregnant after using birth control?
You’re not less likely to become pregnant after you’ve stopped taking birth control. This is true no matter how many years you’ve used the contraceptive. There is no medical evidence that the use of birth control leads to impaired fertility.
It will always vary how long it will take to get back into your "own" menstrual cycle. Some will therefore quickly become pregnant after discontinuing their birth control, while others will need more time.
How do IUDs work?
Intrauterine devices, IUDs, are inserted into the uterine cavity. Pregnancy is prevented since the IUD interferes with the motility of the sperm and prevents any fertilized egg from sticking to the uterine wall.
There are two main types of IUDs; copper IUDs and hormonal IUDs. A midwife or a doctor inserts the IUD. The copper IUD may stay inside the uterus for five years. The typical drawbacks associated with this method include increased menstrual bleeding and cramps.
The hormonal IUD comes in two variants; one that can stay inside the uterus for three years (Jaydess) and the other for five years (Mirena). When using a hormonal IUD, menstrual bleeding will usually be minimal, and possibly become absent. This is a natural effect of the effect of the hormones on the uterine lining (endometrium).
IUDs do not protect against ectopic pregnancy or sexually transmitted infections.
How does a contraceptive implant work?
The implant is a 4 cm thin plastic rod containing the hormone gestagen. The rod is inserted just underneath the skin on the upper inner arm. Local anaesthesia is used before insertion. The rod releases a small amount of hormones daily into the bloodstream.
The hormones prevent ovulation and make the cervical mucous less permeable to sperm. The rod can stay in the arm for three years.
How does the pill work?
Will my sex drive decrease when using contraceptives?
For the vast majority, no. For most people, the use of birth control gives women and couples the opportunity to have an active sexual life without needing to worry about unplanned pregnancies, and the transmission of sexually transmitted diseases (condoms).
Is the "safe period" an effective/safe method of contraception?
No, this is because the time of ovulation can vary considerably.
Is the withdrawal method an effective method?
No, the method is highly uncertain since it is difficult for the man to time his ejaculation. Also, some sperm might “leak” during intercourse. It is not unusual for the man to pull out too late because of the pleasure.
When using birth control, can you be a 100% certain that you won’t get pregnant?
Unfortunately, no, no contraception can guarantee 100% efficacy. That said, today's contraceptives have a very high efficacy rate when used correctly. Long-acting contraceptives such as IUDs and implants (LARC) are the safest methods because there is no risk of user error.
Methods such as birth control pills, contraceptive patches, and condoms, on the other hand, have a higher risk of user error and are therefore less safe.
What is emergency contraception?
The emergency contraceptive pill is an emergency solution that can be used after unprotected sexual intercourse. This pill is actually a mini pill with a high content of the hormone progestin. It delays the production of LH (a hormone), and this will prevent or delay ovulation by about five days.
The pill must be taken as soon as possible or within 72 hours after having had unprotected sex.
What is ovulation, when does it happen, and why is it important?
Every month, hormones in the body contribute to the maturation of some of the millions of cells in the ovaries. At the same time, the uterine lining (endometrium) grows and thickens, and prepares to receive a fertilized egg.
The first egg that matures is released from the ovary. This is ovulation. Most women release one egg at a time. The egg is then caught by the ferny ends of the fallopian tube and is then transported to the uterine cavity. It takes about a day for the egg to get through the fallopian tubes to reach the uterus.
Ovulation occurs about two weeks after the last day of the period, but because women have different lengths of their menstrual cycle, this may vary. On the way through the fallopian tube, the egg might meet the sperm and become fertilized.
Because sperm can live for about 5-7 days, it means that the woman can become pregnant even if she didn’t have intercourse on the day of ovulation. Ovulation is needed to get pregnant!
How big is the chance of getting pregnant on my fertile days?
The "fertile window" is the period in the menstrual cycle where the woman can get pregnant. The sperm cells have a lifespan of up to 5–7 days, while an egg cell will wither and die after 12-24 hours if not fertilized. This means that "the fertile window" extends from around six days before up to 24 hours after ovulation.
It is assumed that there is about a 20% chance of a fertile couple conceiving in one cycle. This will, of course, be individual, and the chances are less after the age of 35.
When can IUDs be inserted after giving birth?
With an IUD insertion, we will consider when it is appropriate to insert it, around 6–12 weeks after birth. There is a small chance of perforation of the uterus with insertion shortly after birth. It may, therefore, be wise to wait 12 weeks after birth but there is no contraindication to inserting IUDs after 6 weeks. After a caesarean section, it is recommended to wait 12 weeks
What contraceptive can I use during breastfeeding?
you want to use hormonal contraception, you should use contraceptives without the hormone estrogen. The most effective are the long-term acting contraceptives (LARC) such as hormonal IUDs, copper IUDs, and contraceptive implants. They are all safe, practical, and affordable methods.
If you want to use birth control pills, you should choose mini-pills/estrogen-free pills; that is, they contain only the hormone gestagen (and not estrogen). Estrogen will negatively affect the mother’s milk production and is therefore not suitable.
Is it true that the chance of breast cancer increases if you’re using birth control pills?
I’ve forgotten a pill - am I still protected from pregnancy?
Oral contraceptives should be taken at approximately the same time each day and within 12 hours, to maintain a steady level of hormones in the blood. If you forget to take as little as one pill, the contraceptive effect will be reduced.
Take the missed pill as soon as possible, and then take the next pill at the usual time. If you have intercourse in the next seven days, you should use a condom to protect against unwanted pregnancy. (It varies slightly depending on which birth control pill you use, always read the package insert).
If you often forget to take your birth control pills, you should switch to another method of contraception such as an IUD or a contraceptive implant (LARC).
What do I do if I vomit after taking the pill?
If you vomit within two hours after taking the birth control pill, take another pill. If you vomit again, do not take more pills, max two per day. You’re still considered safe.
If you experience vomiting or very strong diarrhoea for more than 24 hours, you should use condoms during the following seven days.
Can I switch directly from birth control pills to an IUD and still be safe?
Yes, you can switch from oral contraceptives to copper IUDs at any time as long as you’re actively taking the pills, or at the latest, the seventh day of the pill-free week. You can finish the tray you’re on after the IUD insertion to avoid bleeding disorders.
For the hormonal IUD, complete the tray (21 pills) or skip the placebo pills (28 pills) and insert the hormonal IUD no later than the day after.
Sources
Metodebok , Sex og samfunn- center for young sexual health (The 7th revised issue)
Helsedirektoratet.no (Preventive health care)
“Store norske leksikon”
Long-acting reversible Birth Control (LARC)
The most important principle of contraceptive counselling is that women can choose for themselves. It is essential that women get a wide selection of choices so that they can choose the method that they consider best for themselves.
All of the hormonal contraceptive methods are very safe, and providing excellent protection against pregnancy. Long-acting reversible birth control (LARC); copper and hormonal IUDs and contraceptive implants are the methods that provide the best protection since the probability of user error is small. International knowledge summaries recommend increased use of LARC.
The World Health Organization (WHO) makes the following recommendations on LARC:
Copper IUDs and hormonal IUDs are excellent and easy to use contraceptives. Most women can use them; completely independent of age and whether they have already given birth. The hormonal IUD also appears to have other health benefits such as a decreased risk of pregnancy outside of the uterus (ectopic pregnancy). The copper IUD is a good option for women who, due to medical or other reasons, can’t or don’t want to use hormonal contraception.
Women should, to a much greater extent than is the case today, have options and information on contraception that also includes information about the long-acting contraceptive methods. These methods don’t have the probability of user error, and they have a higher degree of effectiveness against pregnancy than most other methods.
It is the health professional’s responsibility to give the woman information about the LARC methods. It is due to a lack of information that health professionals only recommend this to some groups of women. If you lack experience in inserting IUDs or implant, it is important to refer to another health professional who can do this.
Who can use the LARC methods?
- Women, regardless of whether they have already given birth or not
- Nursing mothers
- Women who have aborted, immediately after
- Women with BMI (body mass index) over 30
- Women with diabetes
- Women with migraine
- Women who should not take estrogen
- Women with HIV
The Norwegian Medicines Agency has created an overview of all the different types of hormonal contraceptive methods with product facts collected together in one guide. The website provides continually updated reviews on birth control as well as an updated overview of contraceptives that can be obtained from health nurses and midwives. It also has recently published articles with current research on, among other things, the use of hormonal methods of birth control.
Public health nurses and midwives can insert implants and IUDs on referral from a doctor, cf. Section 5 of the Health Personnel Act (lovdata.no): ”Health personnel can let another health professional perform specific functions if this is justifiable judging from the nature of the job, the qualifications of the health professional and the follow up given. The assistants or helpers are subject to the supervision of the health professional”.
Useful information
- Recommended hormonal contraceptive methods: legemiddelverket.no
- Checklist and information for prescribers: legemiddelverket.no
- Birth control pills and the risk of blood clots
- Prevention – find your type: sexogsamfunn.no
- The Norwegian Medicines Agency in Norway: legemiddelforbruk.no
- User Manual 2015: sexogsamfunn.no
- Patient info contraception: sexogsamfunn.no
- Other references: Helsedirektoratet.no
What we have to offer
We’re midwives with a long and extensive experience and certification with contraception guidance and insertion of IUD and contraceptive implants.
You can also come to our clinic for an IUD control. It is recommended to have the first check up after three months. Please contact us if you have any questions related to the chosen contraceptive method.
Cheap birth control
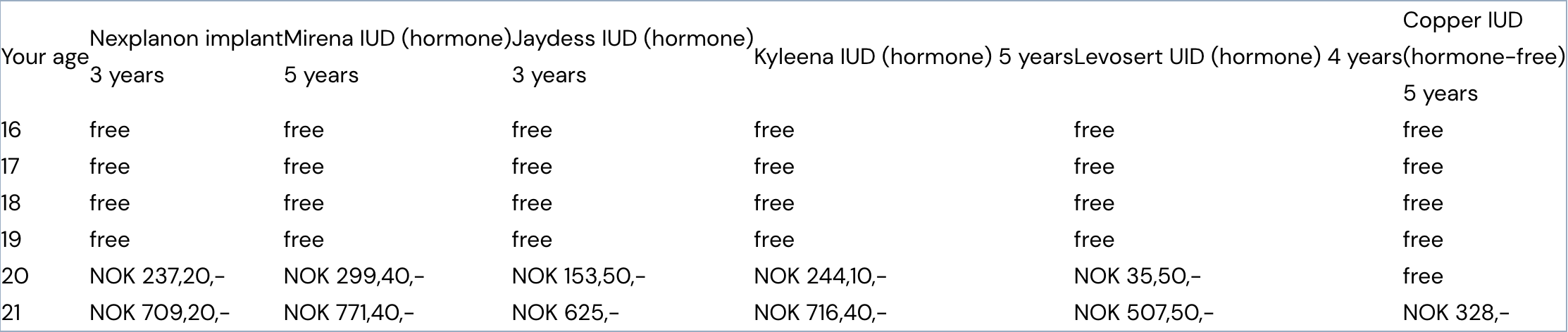
Are you between 16 and 22 years old? The public authorities have created an arrangement for those between the ages of 16 and 22 where you receive financial support for birth control. As of today, this amounts to 118 NOK for 3 months of contraception.
This means that a package with the cheapest pills will be free, and for those that cost more than 118 NOK you have to pay the remaining amount yourself.
If you want a long-term contraceptive (LARC) such as a copper IUD, hormone IUD or a contraceptive implant, the price will depend on how old you are. If you are 16, 17, 18 or 19 all three of them will be free of charge, but if you are 20 or 21 you must pay a deductible.
NB! Only the copper IUD Nova-T 380 is included in the financial contribution scheme. We make sure you get a prescription for the right copper IUD.
You need a prescription to get the IUD from the pharmacy. You can get the prescription from us. Take the prescription with you and buy it at a reduced price at the pharmacy. They will calculate what you will pay in user fee. You can then come back to our clinic with the IUD/implant where we give you information about the contraceptive you have chosen and we can do the insertion.
If you want to use methods other than long-acting contraceptives (LARC), it should always be examined whether it’s medically justifiable to use the contraceptive method. When using combination preparations (like most oral contraceptives are), it should always be examined whether it is medically justifiable for the woman to use the contraceptive. We do this thru what we call anamnesis (medical history). You also get a prescription for the contraceptive method you have chosen.
Below is a table showing the cost of the different methods of long-term contraception.*
Prices given in table valid from 1 January 2019. These are subject to change.
.jpg?width=200&height=117&name=OJUK%20logo_m%20bindestrek%20(002).jpg)